Abstract
Introduction: The Great Recession of 2007-2009 led a new group of families to fall into poverty and took a greater toll on the Black population than other segments of the population. Higher unemployment rates led to increased poverty levels and increased utilization of public insurance.1Given increasing rates of public insurance, we hypothesized that the need for intensive care unit (ICU)-level care at the time of hematologic malignancy diagnosis increased during and following the Great Recession and that this effect is more pronounced among the Black population.
Methods: A retrospective cohort of children with new-onset acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), or mature B cell lymphoma initially treated at free-standing pediatric hospitals between 2004-2013 was assembled from the Pediatric Health Information System (PHIS) administrative database. We defined the primary exposure as the epoch of diagnosis divided into 3 time periods: 2004-2007, 2008-2010, and 2011-2013 based on the plateau in rising unemployment after 2010. The primary outcome was patient acuity at presentation, defined as utilization of ICU-level care in the first 72 hours of the index cancer admission. Proportion of patients with public insurance across epochs was compared using the chi-square test. Logistic regression analyses were used to estimate crude odds ratios (cOR) and corresponding 95% confidence intervals (CI) for acuity by epoch and were subsequently stratified by race to evaluate for effect measure modification.
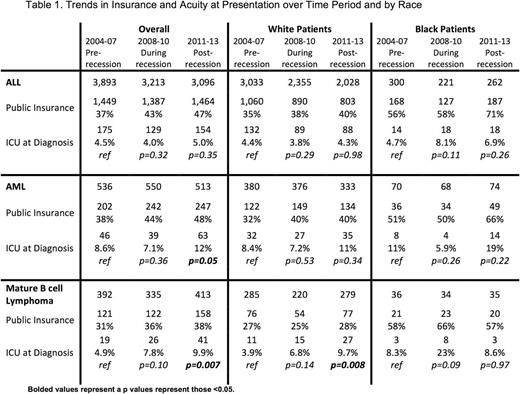
Results: 12,941 patients (10,202 with ALL, 1,599 with AML, and 1,140 with mature B cell lymphoma) were included. Utilization of public insurance across diseases increased from 39% in the Pre-recession period to 47% in the Post-recession period (p <0.0001). In the periods during and after the Great Recession (when compared to the Pre-recession period), ICU-level care increased for AML (During recession cOR 0.81 [95% CI: 0.52, 1.27] and Post-recession cOR 1.49 [95% CI: 0.99, 2.23]) and mature B cell lymphoma (During recession cOR 1.66 [95% CI: 0.90, 3.06] and Post-recession cOR 2.16 [95% CI: 1.23, 3.80]), but not for ALL (During recession cOR 0.89 [95% CI: 0.70, 1.12] and Post-recession cOR 1.11 [95% CI: 0.89, 1.39]) as shown in Table 1. However, among Black patients with ALL, a similar temporal increasing trend in acuity of presentation was observed (During recession cOR 1.81 [95% CI: 0.88, 3.73] and Post-recession cOR 1.51 [95% CI: 0.73, 3.09]).
Conclusions: These data suggest that the Great Recession was associated with increasing acuity of presentation over time for children with AML and mature B cell lymphoma. While the division of patients by time period reduces sample size and thereby limits the power of these analyses to detect statistically significant differences, the majority of measures were in the hypothesized direction and approached or reached statistical significance. The temporal trend of increasing rates of illness acuity among pediatric cancer patients at diagnosis highlights the potential negative healthcare consequences of a recession on economically vulnerable populations.
1Anthony EK, King B, Austin MJ. Reducing child poverty by promoting child well-being: Identifying best practices in a time of great need. Children and Youth Services Review. 2011;33:1999-2009.
Fisher: Merck: Research Funding; Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.